Syphilis, a well-known sexually transmitted disease, unfolds in distinct stages with symptoms that evolve over time. The initial sign is often a painless sore known as a chancre, which can appear at the site of infection. Understanding these stages is crucial for effective intervention and treatment.
Secondary syphilis can present with symptoms like skin rashes and mucous membrane lesions. These may seem innocuous, but they are highly infectious. Some individuals may transition into a latent stage, where symptoms disappear but the bacteria remain active.
If left untreated, the infection can progress to tertiary syphilis, potentially leading to severe health complications. Long-term effects include organ damage and neurological disorders, underscoring the need for timely diagnosis and medical intervention.
OVERVIEW OF SYPHILIS
Syphilis is a sexually transmitted infection caused by a specific type of bacteria. It progresses through various stages and can lead to serious health issues if untreated. Understanding how it spreads and its prevalence can help in its prevention and management.
ETIOLOGY AND TRANSMISSION
Syphilis is caused by the bacterium Treponema pallidum. The primary mode of transmission is through sexual contact, including oral, vaginal, and anal sex. The infection spreads via direct contact with syphilis sores, commonly found on the genitals, rectum, or mouth. It can also be transmitted from a pregnant person to their baby, potentially leading to congenital syphilis.
In rare cases, the infection may spread through blood transfusion. Awareness of its transmission routes can facilitate prevention efforts. Direct contact remains the most significant risk for acquiring the infection, emphasizing the importance of safe sexual practices.
EPIDEMIOLOGY
Syphilis has seen varying prevalence rates worldwide, with certain populations experiencing higher rates of infection. It is crucial to understand the demographic and geographic factors influencing these rates. Men who have sex with men and individuals with multiple sexual partners are at greater risk.
In some regions, public health efforts have managed to reduce syphilis rates, yet periodic outbreaks continue to occur. Monitoring and reporting cases help in developing strategies to combat its spread. The Centers for Disease Control and Prevention and other health organizations play a key role in tracking syphilis trends and tailoring interventions to affected communities.
SYMPTOMS AND STAGES
Syphilis, a sexually transmitted disease, progresses through four distinct stages: primary, secondary, latent, and tertiary. Each stage presents unique symptoms and challenges, requiring careful attention and timely treatment.

PRIMARY STAGE
In the primary stage, syphilis exhibits its initial symptom, a small sore known as a chancre. This typically appears at the site of infection, such as the genitals, anus, or mouth, within two to twelve weeks following exposure. Though the chancre is usually painless and heals on its own, it marks an important phase where the disease is highly contagious.
The chancre may be singular or multiple, presenting a definite risk of transmission during sexual contact. Testing and early treatment during this stage are crucial to preventing progression to later stages.
SECONDARY STAGE
During the secondary stage, syphilis manifests in more systemic symptoms. A distinctive rash, often reddish-brown, can appear on the palms of the hands and soles of the feet. Other symptoms may include fever, swollen lymph nodes, sore throat, and patchy hair loss.
These symptoms, though they may seem mild or flu-like, indicate that the infection is spreading. Without treatment, the disease can transition into a more advanced stage. This is a critical period for receiving medical attention as the individual remains highly contagious.
LATENT STAGE
The latent stage is somewhat deceptive, as it presents without visible symptoms. During this period, the infection lies dormant, remaining inactive for years. The absence of symptoms does not mean the disease is cured but rather that it is quietly progressing internally.
Despite the lack of symptoms, individuals can still harbor the bacteria. It’s possible for the condition to return in a more severe form, emphasizing the need for continued monitoring and treatment if required.
TERTIARY STAGE
Tertiary syphilis is the most severe stage, potentially occurring years after the initial infection. It can affect multiple organ systems, leading to serious complications like neurological disorders, cardiovascular issues, and problems with bones and tissues.
Symptoms may include difficulty with coordination, paralysis, and damage to internal organs. This stage highlights the importance of early detection and treatment to prevent such severe outcomes. While less common due to advancements in diagnosis and care, tertiary syphilis remains a critical concern.
DIAGNOSIS OF SYPHILIS
Diagnosing syphilis involves a combination of physical examinations, laboratory tests, and neurological assessments. Each approach provides critical information required to identify the infection accurately and evaluate its stage.

PHYSICAL EXAMINATION
A comprehensive physical examination is the initial step in diagnosing syphilis. Healthcare providers look for symptoms such as chancres, rashes, or lesions, which are indicative of the disease. Chancres, often painless, can appear on the genitals, mouth, or anus, signaling primary syphilis.
Secondary stage symptoms may include skin rashes and mucous membrane lesions. These signs are crucial as they help establish the spread and phase of the infection. Close inspection of these physical markers aids in narrowing down further diagnostic requirements, informing subsequent laboratory testing and assessments.
LABORATORY TESTING
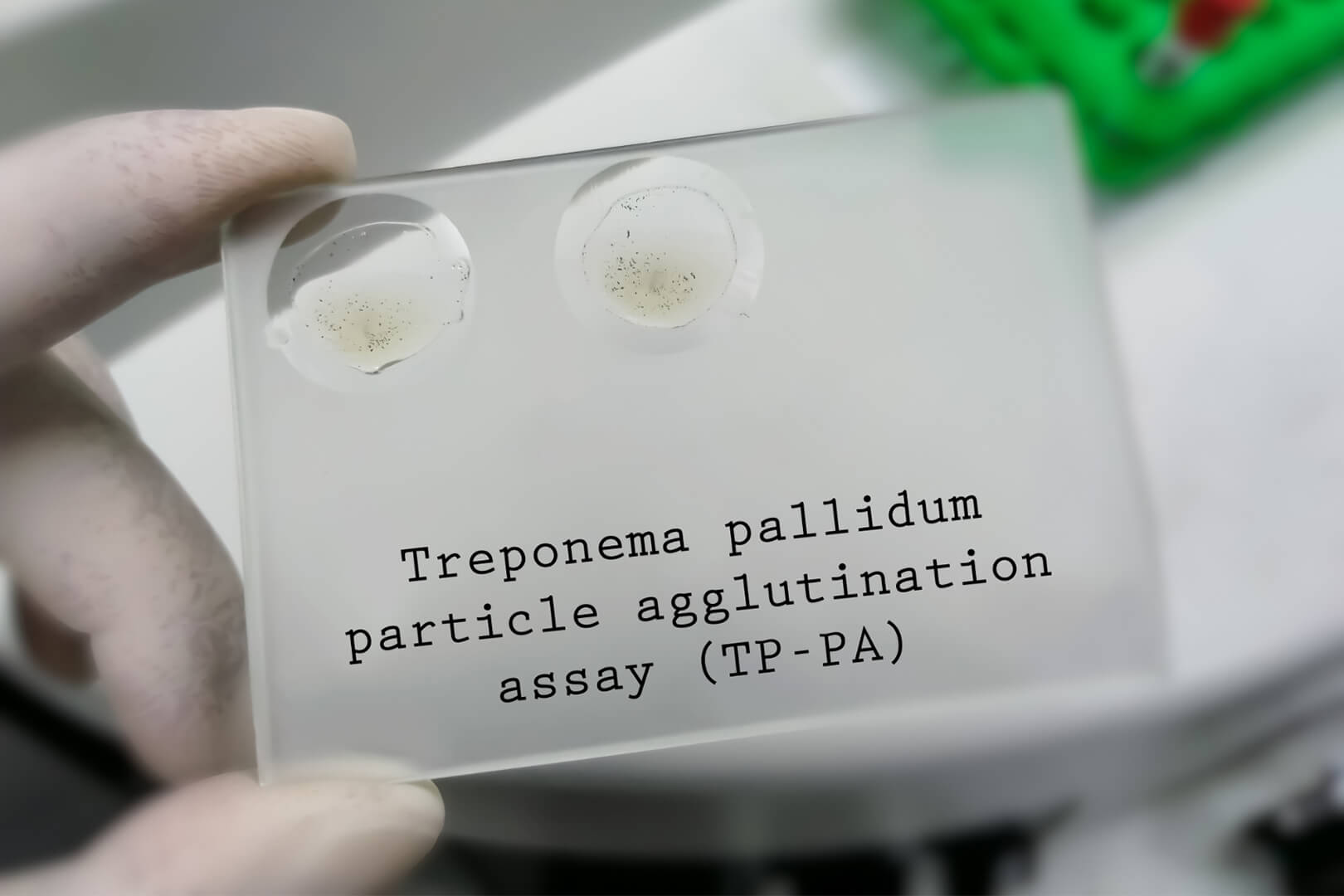
Laboratory tests play a pivotal role in confirming the presence of syphilis. Blood tests such as the VDRL and RPR are used to detect syphilis antibodies, confirming active or past infections. More specific tests like the FTA-ABS and TPPA help differentiate syphilis from other conditions by identifying syphilis-specific antibodies.
These tests are reliable methods for confirming both current and previous infections, particularly when physical symptoms are not evident. Accurate timing and the right choice of tests improve diagnostic certainty, directing appropriate treatment strategies.
NEUROLOGICAL ASSESSMENT
In cases of long-standing or untreated syphilis, a neurological assessment may be necessary. This involves evaluating symptoms of neurosyphilis, a condition where syphilis affects the nervous system. Symptoms can include headaches, altered mental status, or sensory deficits.
A lumbar puncture is often performed to analyze cerebrospinal fluid, checking for the presence of syphilis bacteria or indicators of neurological involvement. Prompt diagnosis through neurological assessments is crucial in preventing irreversible damage and guiding effective treatment to manage this potentially severe complication.
TREATMENT STRATEGIES
Treating syphilis effectively requires a combination of medical interventions and careful monitoring. Antibiotic therapy is the primary approach, accompanied by follow-up protocols and partner treatment to prevent reinfection and further spread.

ANTIBIOTIC THERAPY
Benzathine penicillin G is the standard treatment for all stages of syphilis. It is administered via intramuscular injection, with dosage and frequency varying by stage.
For individuals allergic to penicillin, alternatives include doxycycline or tetracycline. These should only be used after consulting with a healthcare professional due to potential side effects and reduced efficacy compared to penicillin. In specific cases, particularly neurosyphilis, intravenous penicillin is required.
Rapid treatment implementation prevents complications and alleviates symptoms.
MONITORING AND FOLLOW-UP
Regular follow-up is crucial to evaluate treatment success and detect any recurrence. Patients should undergo serologic testing at 6 and 12 months post-treatment, which measures antibody levels.
Decreasing titers typically indicate successful treatment. HIV co-infection may alter the disease course, requiring more frequent monitoring. A sustained elevation or increase in antibody titers after treatment could necessitate a repeat course of antibiotics.
Healthcare providers should educate patients on recognizing symptom changes to ensure prompt medical attention if necessary.
TREATMENT OF SEXUAL PARTNERS
Encountering syphilis in a patient mandates the treatment of recent sexual partners. The Centers for Disease Control and Prevention recommend evaluating and treating partners from the preceding 90 days, even if asymptomatic.
Partner notification services can assist in informing partners and facilitating their evaluation and treatment. While partners typically receive empirical antibiotic therapy, testing can help confirm if they are also infected.
Addressing both patient and partner treatment reduces reinfection risks and helps control the broader spread of syphilis. Clear communication between healthcare providers and patients is essential throughout this process, fostering effective prevention and care strategies.
PREVENTION AND PUBLIC HEALTH
Syphilis prevention focuses on safe sexual practices, comprehensive screening programs, and ongoing efforts in vaccine development. Each plays a crucial role in reducing transmission and managing public health risks associated with this sexually transmitted infection.

SAFE SEX PRACTICES
Engaging in safe sex practices is vital for reducing the risk of syphilis. Use of condoms and dental dams during oral, vaginal, and anal intercourse is recommended, as these barriers reduce exposure to infected fluids. Educating individuals on the importance of limiting sexual partners and maintaining open communication about STI testing with partners can further diminish transmission risks. Regular STI testing for sexually active individuals is also imperative.
Educational programs targeting communities with higher rates of syphilis can increase awareness and promote healthier choices. These initiatives emphasize the importance of prevention tools and widely accessible resources. Furthermore, healthcare providers play a critical role in counseling patients on the importance of protection methods.
SCREENING PROGRAMS
Screening programs are a cornerstone of syphilis management, enabling early detection and treatment. Public health initiatives frequently offer free or low-cost testing to ensure accessibility for all, particularly in high-prevalence areas. Testing is crucial for pregnant women as untreated syphilis can lead to congenital syphilis, impacting the baby’s health.
Implementation of routine screening in healthcare settings catches asymptomatic cases, interrupting transmission chains. Through targeted programs focusing on populations at higher risk, such as MSM (men who have sex with men) and people with HIV, health systems enhance program outcomes. Confirmatory testing following initial screenings ensures accurate diagnoses and appropriate treatments.
VACCINE DEVELOPMENT
While no syphilis vaccine currently exists, research is ongoing. Vaccine development is challenging due to the complexities of the bacterium Treponema pallidum and its variable surface proteins. Scientists are actively working to identify possible antigens that could trigger an effective immune response.
Progress in vaccine research could revolutionize syphilis prevention by providing long-term protection and significantly reducing infection rates. Funding and collaborative efforts among global health organizations bolster research aiming to bring a vaccine to market. Such a breakthrough could have a considerable impact on curbing syphilis prevalence and progressing public health goals worldwide.

